Written By: Jennifer Kinkade, OTD, OTR
Evidence-based practice (EBP) is necessary and expected within the allied health professions. Did you know there is a 17-year gap in knowledge-to-practice when it comes to allied health practitioners implementing evidence? The reality is that many encounter barriers that make it difficult to do implement EBP successfully.
 What is Evidence-based Practice (EBP)?
What is Evidence-based Practice (EBP)?
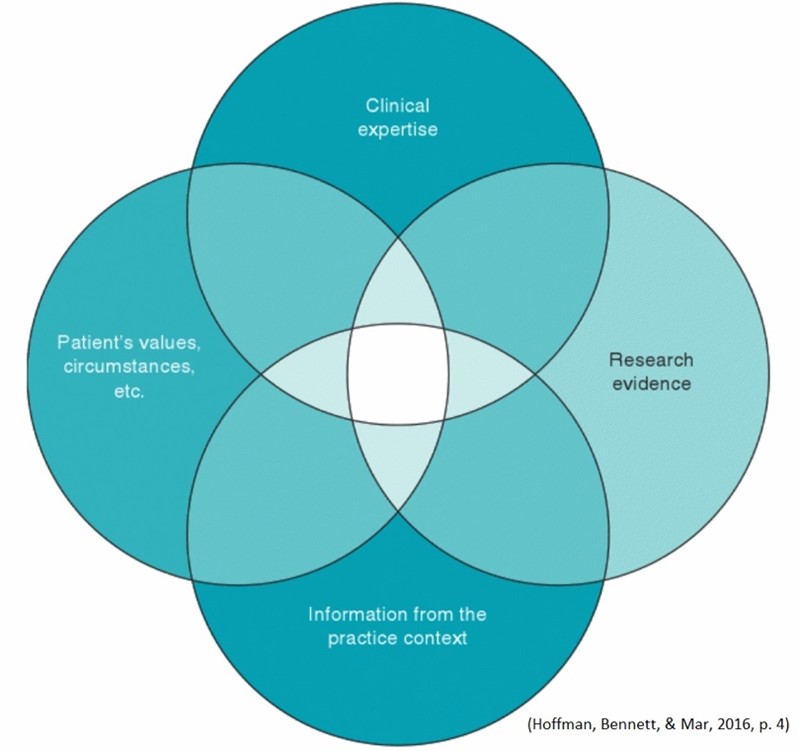
Evidence-based practice is a process that combines the best research evidence, clinical expertise, client experiences and practice context. Integrating all four of these components allows practitioners to make informed, evidence-based decisions and provide quality services promoting positive outcomes.
Three Common Barriers to Implementing EBP
The three most common barriers to implementing EBP are:
- Lack of Awareness & Education
- Time Constraints
- Lack of Organizational Support
Lack of awareness and education encompasses limited knowledge about what EBP is and limited access to reliable resources. Practitioners have varied understanding of what EBP includes. It is a common misconception that EBP relates to only the research around a particular topic.
The issue of time constraints is familiar to many. Whether one carries a large caseload, works long hours, or has conflicting priorities in other areas of life, time can be a barrier when it comes to implementing EBP.
Lack of organizational support is apparent in different ways. Restrictive budgets and limited administrative support are two barriers that cause practitioners to rely on traditional methods of intervention rather than those based on evidence.
Active Strategies to Increase the Use of EBP in Practice
Identifying the barriers one experiences is an important first step to improving implementation of EBP. Once the barriers are clear, active strategies can be used to increase EBP uptake.
- Develop mentoring opportunities
- Designate EBP champions in the workplace
- Participate in collaborative experiences
- Educate team members about the importance of EBP
- Attend workshops and continuing education related to EBP
- Start a journal club within your practice community
- Use evidence maps and other tools to document acquired evidence
- Take advantage of resources related to EBP provided by your professional organization
- Contact your alma mater to inquire about library access
- Adopt time management strategies and prioritize a time to explore recent research
The use of evidence-based practice aligns with professional expectations, improves quality of care, promotes positive outcomes, and reduces healthcare costs. Identifying barriers and employing active strategies are the first two steps toward improved use of EBP. If you would like to dive into this topic further, register for my upcoming Summit Live Webinar, Integrating Evidence-Based Practice (EBP), on September 13th. This course will focus on strategies for understanding scholarly articles for any discipline or topic. Participants will learn how to identify relevant evidence through critical appraisal of journal articles. Hope to see you there!
Visit summit-education.com for more information.
References:
Hoffmann, T., Bennett, S., & Del Mar, C. (2016). Evidence-based practice across the health professions (3rd ed.). Elsevier Australia.
Moore, J.L., Carpenter, J., Doyle, A.M., Doyle, L., Hansen, P., Hahn, B., … Van Der Laan, K. (2018). Development, implementation, and use of a process to promote knowledge translation in rehabilitation. Archives of Physical Medicine and Rehabilitation, 99(1), 82-90. doi: 10.1016/j.apmr.2017.08.476
Scott, S. D., Albrecht, L., O’Leary, K., Ball, G. D., Dryden, D. M., Hartling, L., . . . Klassen, T. P. (2011). A protocol for a systematic review of knowledge translation strategies in the allied health professions. Implementation Science,6(1). doi:10.1186/1748-5908-6-58
Weiss, D., Tilin, F., & Morgan, M. (2017). The interprofessional health care team: Leadership and development, (2nd ed.). Jones & Bartlett Learning.

Excellent discussion!
Organizational support is so critical to enabling staff to embed these practices into daily work.