Written By: Michelle Millner, PT, DPT, OCS, CMTPT
 Decreased core strength is associated with a decrease in postural stability, decreased function, and increased fall risk in older adults. These types of weaknesses can be progressive over time due to age-related changes including sarcopenia. As rehab professionals, treating these weaknesses and functional limitations is our bread and butter. Unfortunately, patient compliance with “core” exercises is often limited in our older population. I’ve been fortunate enough to practice PT for over 15 years and I’ve learned that the key to success with core exercises can be broken down into three main categories. The first is to ensure that the patient fully understands the problem and the solution. Essentially, the patient needs to “buy in” to the treatment plan and be willing to participate in the program. Second, treatment needs to be specific to the problem the patient is trying to solve. Performing seated hip adduction exercises when a patient wants to stand up straighter, just doesn’t correlate. A patient will not believe the exercise will help because it is not relevant to the problem. Third, the treatment needs to progress to a functional application as soon as possible. This ensures that the patient sees progress and relevancy.
Decreased core strength is associated with a decrease in postural stability, decreased function, and increased fall risk in older adults. These types of weaknesses can be progressive over time due to age-related changes including sarcopenia. As rehab professionals, treating these weaknesses and functional limitations is our bread and butter. Unfortunately, patient compliance with “core” exercises is often limited in our older population. I’ve been fortunate enough to practice PT for over 15 years and I’ve learned that the key to success with core exercises can be broken down into three main categories. The first is to ensure that the patient fully understands the problem and the solution. Essentially, the patient needs to “buy in” to the treatment plan and be willing to participate in the program. Second, treatment needs to be specific to the problem the patient is trying to solve. Performing seated hip adduction exercises when a patient wants to stand up straighter, just doesn’t correlate. A patient will not believe the exercise will help because it is not relevant to the problem. Third, the treatment needs to progress to a functional application as soon as possible. This ensures that the patient sees progress and relevancy.
Let’s walk through an example of this process in an outpatient clinic:
A 70-year-old female comes into the clinic with complaints of upper back/neck pain, and she is having trouble keeping her head up when sitting, standing, and walking. Step 1 is to make sure she understands the relationship between upper back strength and posture. She may need some education regarding the impact of thoracic spine and scapular strength.
Step 2 is to prescribe exercises that are focused on improving trunk extension strength may be appropriate to prescribe. While these exercises are not functional, they are targeted to the specific area in question.
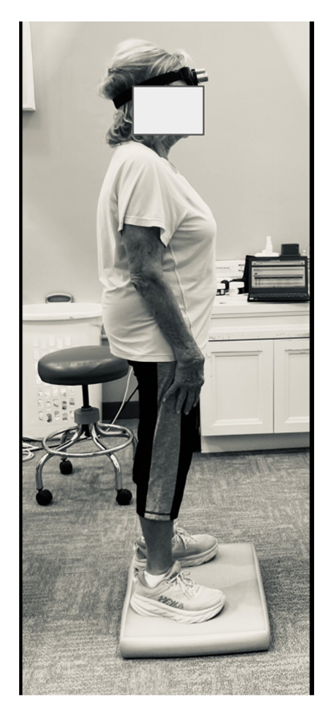
Step 3 is to transition these specific exercises to a functional task. In this case, her goal is to stand and walk without looking down as much. She was instructed to work on a standing exercise with a laser feedback tool while performing gaze and balance tasks. This translates well into her functional daily life.
By following this sequence, most patients will be more motivated to actively participate in their rehabilitative process and therefore make more progress towards their own functional goals.
Interested in learning more? Register for my upcoming Live Webinar on April 23rd, Improving Core Strength and Posture in Older Adults. One-third of people over the age of 65 fall every year. Loss of core and extremity strength may be contributing factors to postural changes, decreased function, and fall risk in older adults. This course provides clinicians with simple and effective tests and measures to assess patients quickly in most clinical environments. By utilizing these strategies, therapists will be able to establish baseline measures of function and track progress through a plan of care. Additionally, clinicians will be able to use these measures as a foundation for building focused exercise programs. Can’t make it? No worries! You can watch this course at any time here.
Explore online continuing education courses from Michelle below:
Improving Core Strength and Posture in Older Adults Part 1: Assessments
Improving Core Strength and Posture in Older Adults Part 2: Exercise Prescription
Evidence-Based Differential Diagnosis and Clinical Reasoning For Unusual Cases of the Spine
Visit summit-education.com for more information.
About Summit Professional Education
Summit equips therapists with better continuing education courses that provide CEUs while impacting patient outcomes. Find high-quality on-demand CE along with the largest offering of live options — including live webinars, live streams, and in-person courses. Want to deep dive on a topic? Summit offers hundreds of 6-hour courses for the most in-depth learning!