Written By: Dana Davis, PT, DPT, CWS
 Despite personally working in the field of wound care as a physical therapist for over a decade, I still believe it is an up-and-coming field of therapy in which we can learn so much and improve our patient outcomes. We as therapists are making headway in this field and could be a crucial piece to a chronic wound patient’s care paradigm. Often wounds are overlooked, given antibiotics and kept covered with gauze (sometimes left open to “air it out”)!
Despite personally working in the field of wound care as a physical therapist for over a decade, I still believe it is an up-and-coming field of therapy in which we can learn so much and improve our patient outcomes. We as therapists are making headway in this field and could be a crucial piece to a chronic wound patient’s care paradigm. Often wounds are overlooked, given antibiotics and kept covered with gauze (sometimes left open to “air it out”)!
So, when you are faced with a wound that just isn’t behaving “as expected” it’s time to take a deeper look into what is causing this wound to occur. Any wound that is open for greater than 4 weeks is considered a chronic wound. It would do a great service to our patients if we took the time to learn more about chronic wounds and not ignore this injury to their largest organ of their body.
 When wounds do not move through a typical healing cascade timeline, there’s always a reason. First things first, collect a thorough history! We need to investigate the cause of this wound. How is their vascular flow? Was there trauma? Note: just because there is trauma doesn’t mean this is a straightforward wound. There is a reason why this wound is not healing well. When trauma is involved, consider foreign objects, infections and comorbidities. IF there are red flag comorbidities such as autoimmune disorders, family history of wounds, chronic wounds, etc you may start to consider an atypical etiology.
When wounds do not move through a typical healing cascade timeline, there’s always a reason. First things first, collect a thorough history! We need to investigate the cause of this wound. How is their vascular flow? Was there trauma? Note: just because there is trauma doesn’t mean this is a straightforward wound. There is a reason why this wound is not healing well. When trauma is involved, consider foreign objects, infections and comorbidities. IF there are red flag comorbidities such as autoimmune disorders, family history of wounds, chronic wounds, etc you may start to consider an atypical etiology.
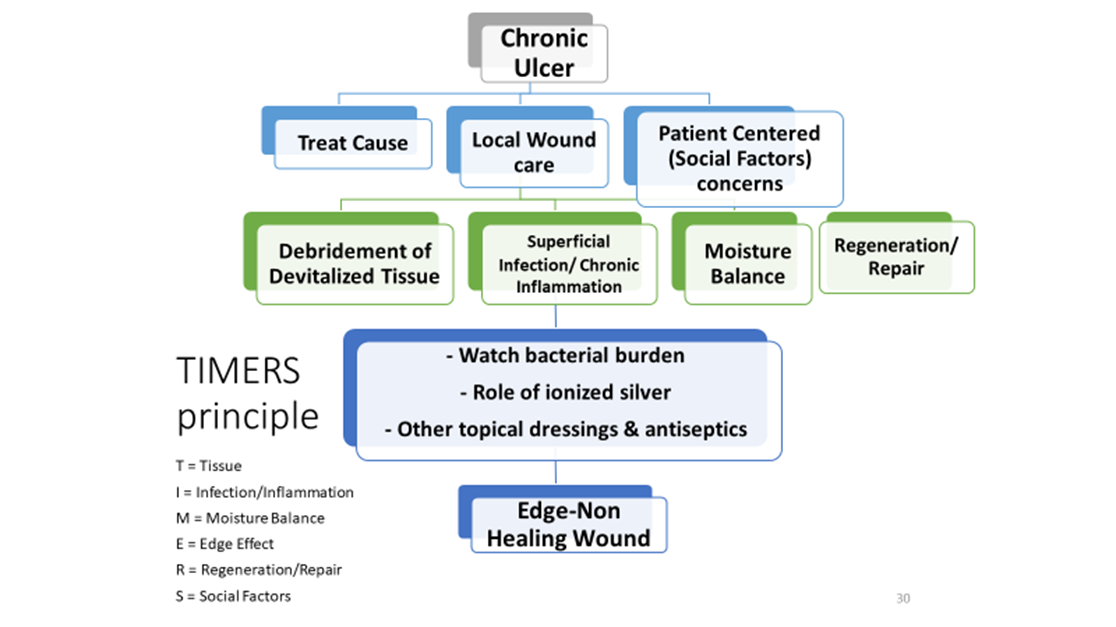
You may wonder, why is that important to know what is CAUSING the wound? Aren’t we just treating the wound and covering it back up? As a therapist we never just treat one symptom. If a patient with back pain presents in your clinic, don’t you take a look at their ENTIRE body? Check their core strength, hips etc? SAME goes with wound care, we need to treat the entire body and knowing the cause of a wound tells us a great deal.
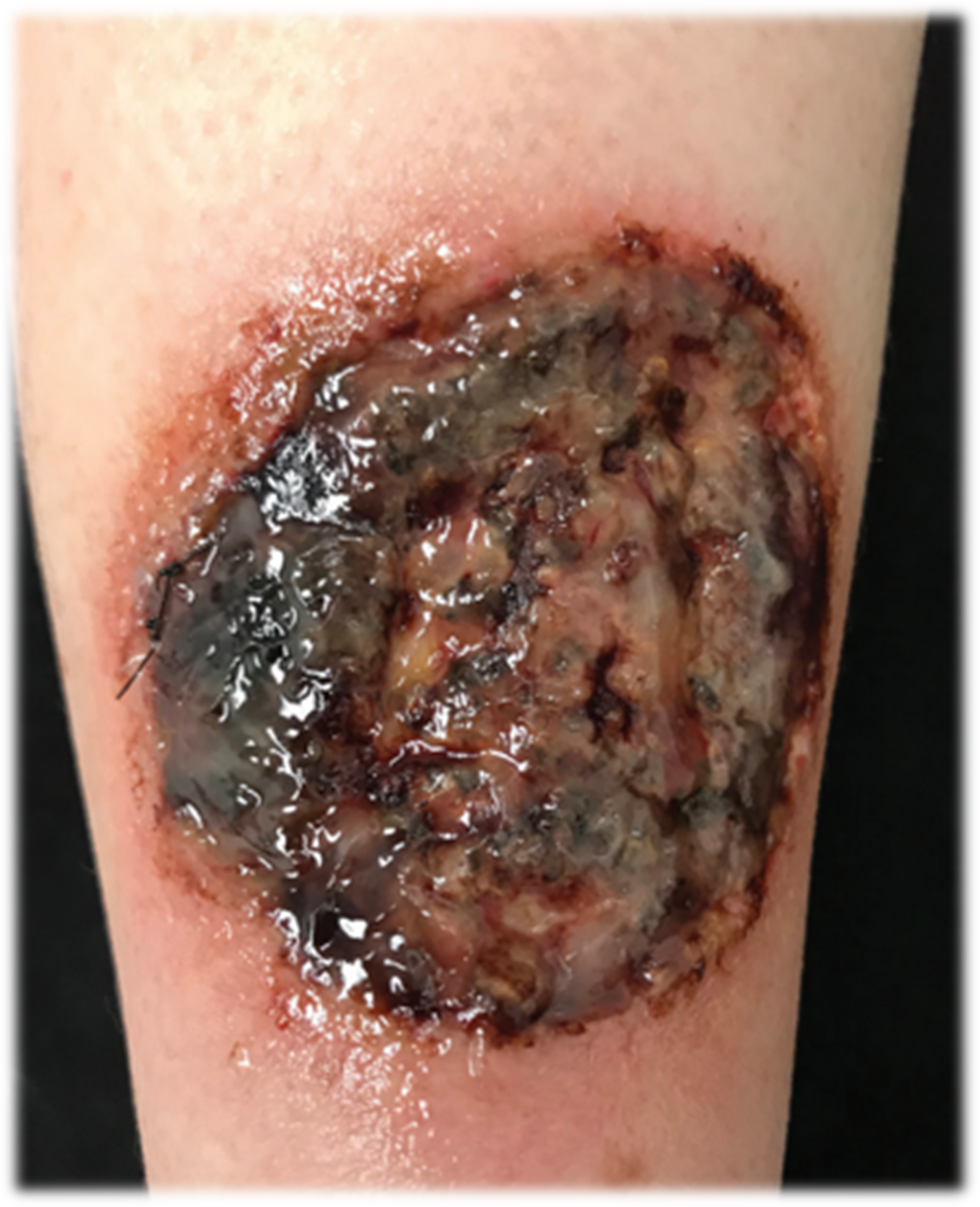
Some atypical wounds, were you to proceed to treat as you would a chronic venous wound, diving into debridement quickly, may cause enlargement.
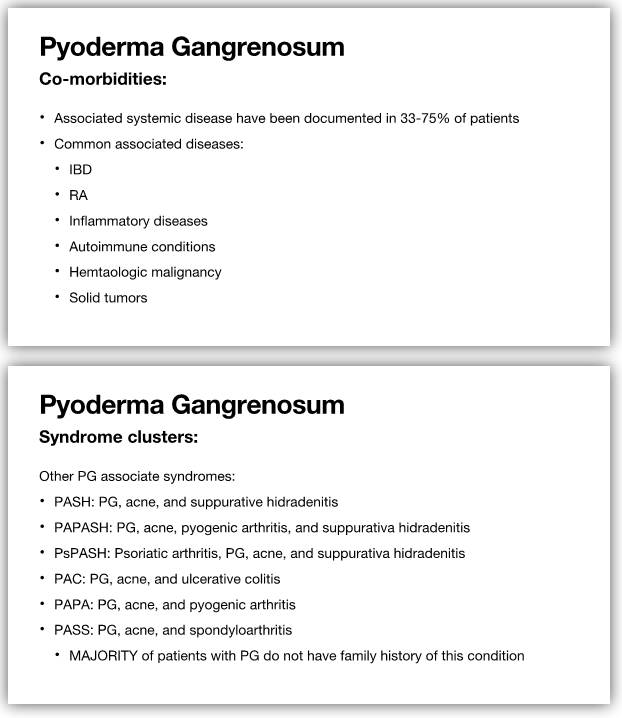
Pyoderma Gangrenosum is a great example of this situation. If treated as a traumatic wound, a physician may choose to take the patient to the OR for debridement since their pain level is so high. A surgical debridement can cause this wound to rapidly increase in size. Though these wounds are frequently initiated due to trauma, with a presentation of significant necrotic tissue and presumed elevated bioburden, they are NOT progressing down a typical pathway for healing. If you take the time for a thorough history and look closely at the patient’s comorbidities often IBD, Crohn’s disease and RA are highly correlated with PG. These would jump out at you as a treating clinician as red flags for further investigation. A diagnosis of PG would change your treatment plan drastically to a more conservative approach from a therapeutic debridement standpoint and as a therapist we would be seeking prescriptions for steroids or medical intervention for this patient.
Join me for my upcoming Live Webinar, Atypical Wounds, as I dive into several other atypical wounds that are commonly seen in the wound therapy setting and learn about the pathophysiology, presentation and clinical signs and symptoms of these diagnoses, along with the most up-to-date treatment approaches to manage these patients.
Explore online continuing education courses from Dana below:
Evidence-Based Edema, Skin, and Wound Care
Wound Composition and Assessment
Visit summit-education.com for more information.
References:
Pyoderma Gangrenosum: A Critical Appraisal. Shavit, Eran MD; Alavi, Afsaneh MD, MSc, FRCPC; Sibbald, R. Gary MD, DSc (Hons), MEd, BSc, FRCPC (Med)(Derm), FAAD, MAPWCA Author Information Advances in Skin & Wound Care: December 2017 – Volume 30 – Issue 12 – p 534-542 doi: 10.1097/01.ASW.0000526605.34372.9e
George C, Deroide F, Rustin M. Pyoderma gangrenosum – a guide to diagnosis and management . Clin Med (Lond). 2019;19(3):224-228. doi:10.7861/clinmedicine.19-3-224
Ulcerative pyoderma gangrenosum Megan Sander DMD, Michael Sander MD n Cite as: CMAJ 2019 September 23;191:E1058. doi: 10.1503/cmaj.190721
Androutsakos T, Stamopoulos P, Aroni K, Hatzis G. A case report of successful treatment of pyoderma gangrenosum in a patient with autoimmune hepatitis, and review of the literature. BMC Gastroenterol. 2015;15:149. Published 2015 Oct 26. doi:10.1186/s12876-015-0376-1